Overview
The cervical spine or neck region is a complex entity of interconnecting bones (vertebrae), mobile joints, nerves, ligaments, and muscles all working together to provide support, stability and flexibility, especially on extending, bending and rotation. Injury to any of these structures in the cervical spine can lead to neck pain. A lot of times the pain is triggered by more than one structure, making the source difficult to identify.
Chronic neck pain is a chronic pain syndrome in the cervical region lasting for at least 3 months. It represents a common problem that severely impairs the quality of life.
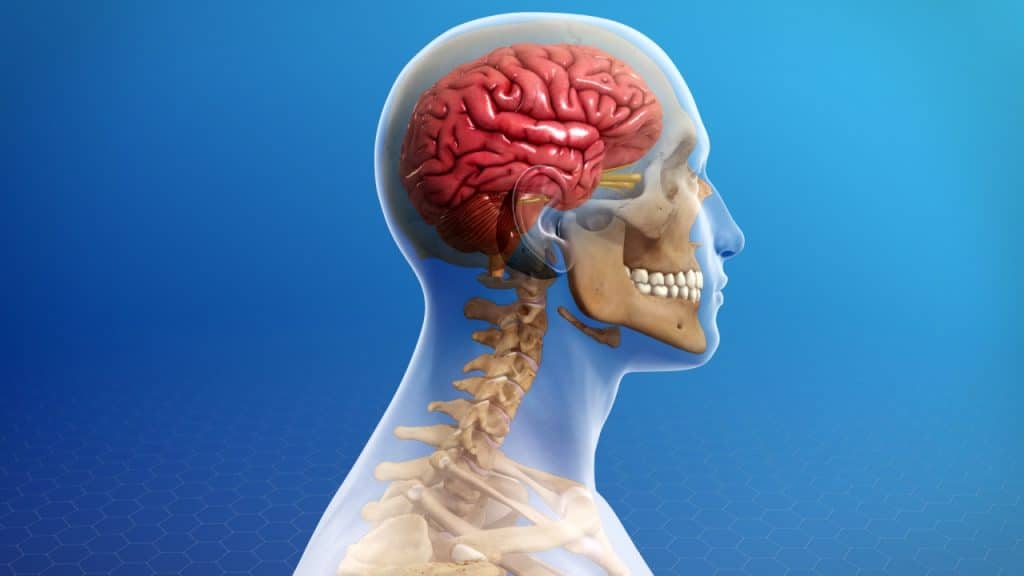
Anatomy (Neck Anatomy)
The neck anatomy is a well-engineered structure of bones (vertebrae), nerves, muscles, ligaments and tendons. The cervical spine consists of seven vertebrae, which are the smallest and uppermost in location within the spinal column and supported by strong ligaments and several muscles. The cervical vertebrae connect the neck to the thoracic spine (the upper back). All seven vertebrae are numbered. The C1, the first vertebra in the column (closest to the skull), is also known as the atlas. The C2, the vertebra below it, is also known as the axis. The C stands for cervical.
Anatomy (The Atlanto-Occipital Joint)
This joint is where the lower part of the occipital bone (base of the skull) connects with the first cervical vertebra, called the atlas. This region facilitates the passing of the spinal cord out of the skull and down into the cervical spine.
Anatomy (Intervertebral Discs)
The intervertebral discs are shock absorbers that are located between the bones of the spine, called vertebrae (hence the name intervertebral). They are designed to help the back stay flexible while resisting forces and to allow bending, flexion and twisting of the spine. Each disc has a thick outer layer, known as annulus fibrosus, that surrounds the soft gel-like center, known as nucleus pulposus. A herniated disc occurs when the jelly-like material inside the disc nucleus herniates or leaks out of the disc and presses on an adjacent nerve root.
Anatomy (Facet Joints)
The facet joints or zygapophyseal joints are a set of joints between the articular processes of two adjacent vertebrae. They are covered with cartilage and are surrounded by a lubricating capsule that enables the vertebrae to bend and twist. Each capsule has a rich supply of tiny nociceptive nerve fibers and implicates this structure as a potential source of pain. Similar to other joints in the body, the facet joints are vulnerable to inflammation and degeneration.
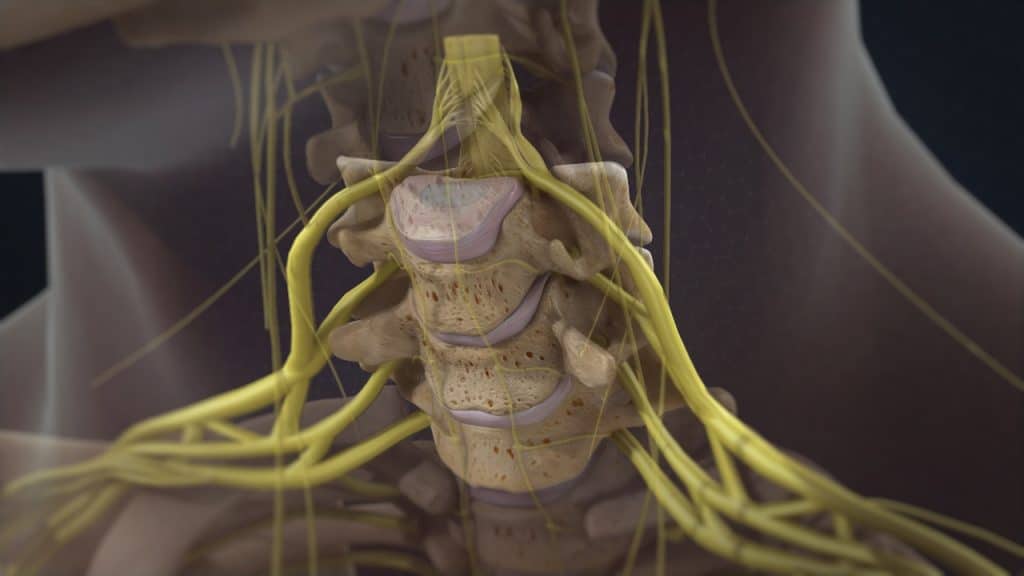
Anatomy (Spinal Nerves)
The entire length of the vertebral column has a large central canal or passage, called the spinal canal. In the cervical and thoracic regions of the spine, the spinal cord descends through this space. In the lumbar region of the spine, this space contains a bundle of nerve roots. Openings or holes to each side of the canal, called the neural foramen (intervertebral foramen – foramen between the two adjacent vertebrae) provide pathways for the nerve roots that travel from the spine to other parts of the body.
Causes
Neck pain is caused due to an underlying joint, disc, muscle, or nerve disorder in the neck. The anatomical structures within the cervical region are interconnected, so an injury to one is likely to affect the health of the others. While acute neck pain is most commonly caused by muscle strain and/or soft tissue sprain such as ligament and tendon sprain, chronic neck pain is often resulting from injury to the facet joints and intervertebral discs in the lower cervical spine.
Common Causes (Muscle Strain and Ligament Sprain)
Neck muscle strain or ligament sprain caused by damage to the muscles and ligaments are the most common causes of neck pain. Strains occur when a muscle is stretched too far and tears, damaging the muscle itself. Sprains occur when over-stretching and tearing affects ligaments, which hold the bones together.
A neck muscle strain and/or ligament sprain can happen suddenly such as by falling or through a sudden impact that pushes the head to the side or by holding the head in an unusual position for a long period, such as having a long conversation while cradling a phone between the neck and shoulder.
A neck muscle strain and/or ligament sprain can also develop slowly over time from repetitive movements such as poor posture. Overuse or disuse of certain neck muscles may result in muscle fatigue or weakness leading to neck pain and discomfort. People who constantly sit with their head in forward and/or downward positions, such as those who do computer jobs on a continual basis, can end up with tight muscles at the back of the head, and eventually can develop neck pain.
Furthermore, certain occupations such as hair stylists and drivers may be at a higher risk for neck pain due to their head posture while working.
Finally, sleeping with the neck at an awkward or atypical position that overextended the neck can lead to neck pain in the morning as well. It is often referred to as a crick in the neck.
Common Causes (Degenerative Disc Disease)
Another common cause of neck pain is a degenerative disc disease. Degenerative disc disease is an age-related condition that happens when one or more of the discs deteriorate or break down, allowing vertebral bones above and below the disc to shift out of position. The bones can touch, pinching nearby nerve roots, leading to pain and possibly accompanying neurological symptoms such as pins-and-needles tingling, numbness, and/or weakness in the areas served by the affected nerve roots.
Common Causes (Cervical Herniated Disc)
Cervical disc herniation is a disease affecting the cervical region that may trigger neck pain. A herniated disc can allow disc material to press harmfully against nearby nerve roots, triggering neck pain and possibly pain and nerve symptoms such as tingling, numbness, and/or weakness that can radiate down into the shoulder, arm, and/or hand.
Common Causes (Facet Joint Disease)
Facet joint syndrome or facet joint disease is a pain arising from the intervertebral joint facets. It occurs when these joints become stressed and damaged. This damage can occur from everyday wear and tear, injury to the back or neck or because of intervertebral disc degeneration and loss of inherent structural integrity.
The cartilage that covers the stressed facet joints gradually wears away. The joints become swollen and stiff. The vertebral bones rub directly against each other, which can lead to growth of bone spurs along the edges of the facet joints and to an enlargement of the joints.
Common Causes (Cervical Osteoarthritis)
Osteoarthritis of the spine develops as a consequence of the natural aging process. It can affect the spine at any level, resulting in pain and discomfort that can grow worse over time.
Cervical spondylosis is a broad term used to describe pain from degenerative conditions of the cervical spine.
Common Causes (Cervical Foraminal Stenosis)
Cervical foraminal stenosis is the most common cause of cervical radiculopathy. When a foramen (bony opening where a nerve root exits the spinal canal) narrows and becomes smaller, the nerve root has less space and may become impinged.
Degenerative changes related to cervical osteoarthritis and/or cervical degenerative disc disease may result in nearby bone spurs (osteophytes), thickening ligaments, or a disc bulging that creates harmful pressure against the nerve root in the foramen.
Common Causes (Cervical Spinal Stenosis)
Spinal stenosis is an abnormal narrowing of the spinal canal (bone channel occupied by the spinal nerves or the spinal cord) or of the neural foramen (bony opening where a nerve root exits the spinal canal). This can cause a compression of the nerves or a compression on the spinal cord, known as cervical myelopathy. Spinal stenosis is often the result of degenerative conditions such as osteoarthritis and/or degenerative disc disease.
Common Causes (Cervical Radiculopathy)
Cervical radiculopathy is a disease involving dysfunction of one or more nerve roots in the cervical spine that typically manifests as pain radiating from the neck into the distribution of the affected nerve root. It can be accompanied by sensory, motor, or reflex disturbances. Any condition that somehow compresses or irritates a cervical nerve root can cause cervical radiculopathy. It most often results from degenerative disease in the cervical spine, but it can also occur due to an acute injury or illness.
Common Causes (Trauma)
Neck pain can be caused by direct trauma to the back of the head or neck. This could be anything from a fall to a car accident or even a sports injury. The facet joints in the cervical spine are prone to injury due to the weight-bearing function they perform while supporting the head. The most common cause of trauma to facet joints is whiplash injury as a result of a motor vehicle accident, resulting in pain shortly after the injury. Neck pain originating from whiplash may resolve in a few days or may last for years.
Symptoms
Depending on the pain generator, symptoms can be experienced in a variety of ways. Neck pain can be mild or so intense to the point that it interferes with daily activities, such as sleep. It can occur suddenly or develop slowly and gradually aggravate over time. Neck pain symptoms might be short-lived, come and go regularly, return intermittently or become constant.
Neck pain is commonly associated with a neck stiffness, which is typically characterized by soreness and reduced range of motion, especially when trying to move the head from side to side.
It can also be accompanied by headache. This could be either a tension headache, as a result of muscle spasms in the neck with tightness or occipital neuralgia, a distinct type of headache, which is caused by irritation or injury of the greater and/or lesser occipital nerves. A cervicogenic headache is a distinct type of headache that occurs when pain is referred from a specific source in the neck up to the head.
In cases of spinal stenosis and cervical herniated disc, an affected spinal nerve in the neck region may result in neck pain and possibly pain and nerve symptoms such as tingling, numbness, and/or weakness that can radiate down into the shoulder, arm, and/or hand.
Neck pain symptoms may be aggravated by certain activities or postures and is often relieved by changing positions.
Treatment
Treatment options for neck pain depend on the source of pain and severity of the injury. Treatment for neck pain is mainly conservative with rest, heat therapy, analgesic/anti-inflammatory medications, muscle relaxants, manual and physical therapy.
Facet joint infiltrations or facet joint blocks may be administered not only to diagnose facet joint pain but also to treat it. If the patient shows a positive response to the facet joint blocks after having failed nonoperative care, the next treatment option is often radiofrequency denervation or rhizotomy.
The cervical radiculopathy can usually be treated successfully without surgery with a combination of pain management techniques, physical therapy and therapeutic spinal injections.
Surgery may be recommended if the conservative therapies do not alleviate pain or if a significant neurologic deficit such as progressive muscle weakness or compression on the cervical spinal cord, known as cervical myelopathy, exists.
References
- Kraemer J., Hasenbring M., Kraemer R., Taub E., Theodoridis T., Wilke H.J.: Intervertebral Disc Diseases: Causes, Diagnosis, Treatment and Prophylaxis. Thieme 2009.
- Theodoridis T., Kraemer J.: Injektionstherapie an der Wirbelsäule. Manual und Atlas. 3. Auflage. Thieme 2017.
- Rhee J., Yoon T., Riew D.: Cervical Radiculopathy. Journal of the American Academy of Orthopaedic Surgeons 2007; 15: 486-494.
- Childress M., Becker B.: Nonoperative management of cervical radiculopathy. American Family Physician 2016; 93(9): 746-754.
- Woods B., Hilibrand A.: Cervical Radiculopathy: Epidemiology, Etiology, Diagnosis, and Treatment. Journal of Spinal Disorders & Techniques 2015; 28(5): 251-259.
- Haldeman S., Dagenais S.: Cervicogenic Headaches. A critical Review. The Spine Journal 2001; 1(1): 31-46.
- Niethard F., Pfeil J., Biberhaler P.: Orthopädie und Unfallchirurgie. 6. Auflage. Thieme 2009.
- Wirth CJ., Mutscher W.: Praxis der Orthopädie und Unfallchirurgie. 2. Auflage. Thieme 2009.