Overview
Osteoarthritis of the spine develops as a consequence of the natural aging process. It can affect the spine at any level, resulting in pain and discomfort that can grow worse over time.
Spondylosis is a broad term used to describe pain from degenerative conditions of the spine.
Degenerative arthritis is the most common cause of low back pain, especially in people over 50.
Anatomy
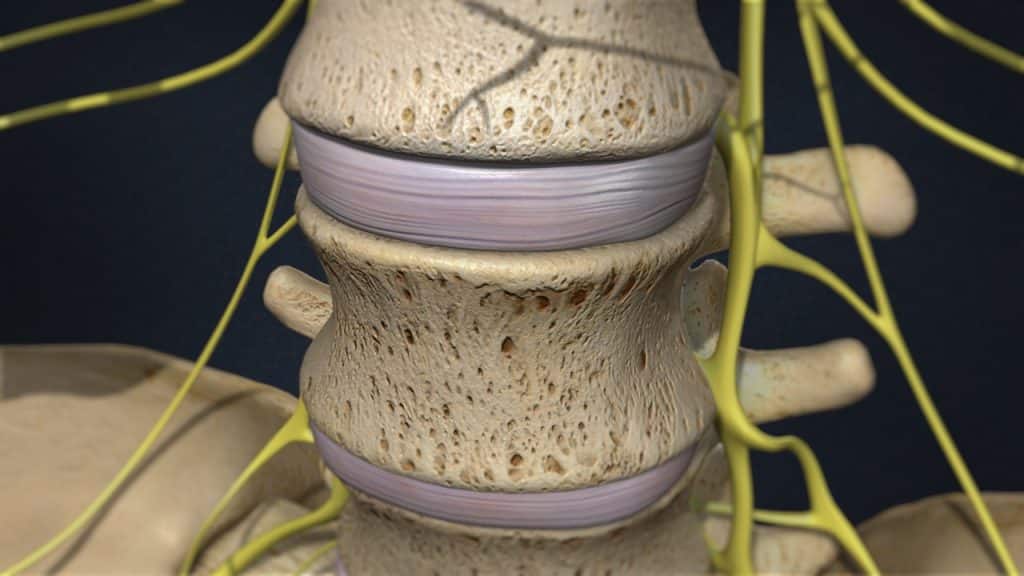
The intervertebral discs are shock absorbers that are located between the bones of the spine, called vertebrae (hence the name intervertebral). A healthy, well-hydrated disc contains a great amount of fluid in its center, known as the nucleus pulposus, which provides cushioning and flexibility to the spine.
The facet joints or zygapophyseal joints are a set of joints between the articular processes of two adjacent vertebrae. They are covered with cartilage and are surrounded by a lubricating capsule that enables the vertebrae to bend and twist. Each capsule has a rich supply of tiny nociceptive nerve fibers and implicates this structure as a potential source of pain. Similar to other joints in the body, these joints are vulnerable to inflammation and degeneration.
Degeneration Process
The degeneration process usually begins with the discs – Disc Degeneration:
1.Loss of Fluid
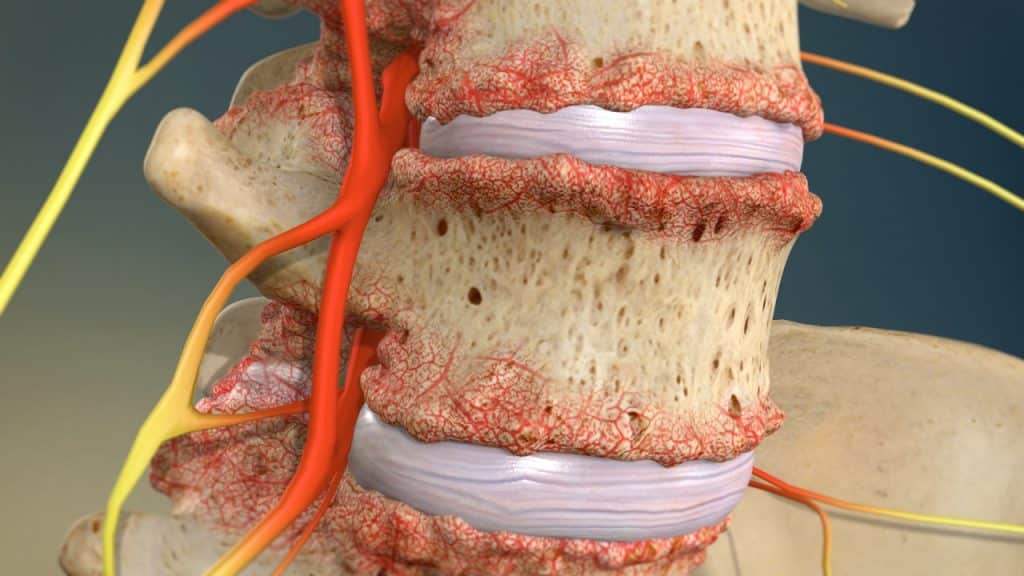
A degenerated disc is marked by a significant decrease in hydration, making the disc less flexible, thinner with narrowing the distance between the adjacent vertebrae, and more prone to tearing or cracking in the outer layer of the disc (disc wall), known as annulus fibrosus.
2. Disc Tearing – Disc Healing – Disc Weakening and Collapse
The disc is unable to truly repair itself because it does not have a direct blood supply. Consequently, a tear in the annulus either will not heal or will develop a scar tissue that is not as strong as the original one, having the potential to break again with further disc-weakening and collapse.
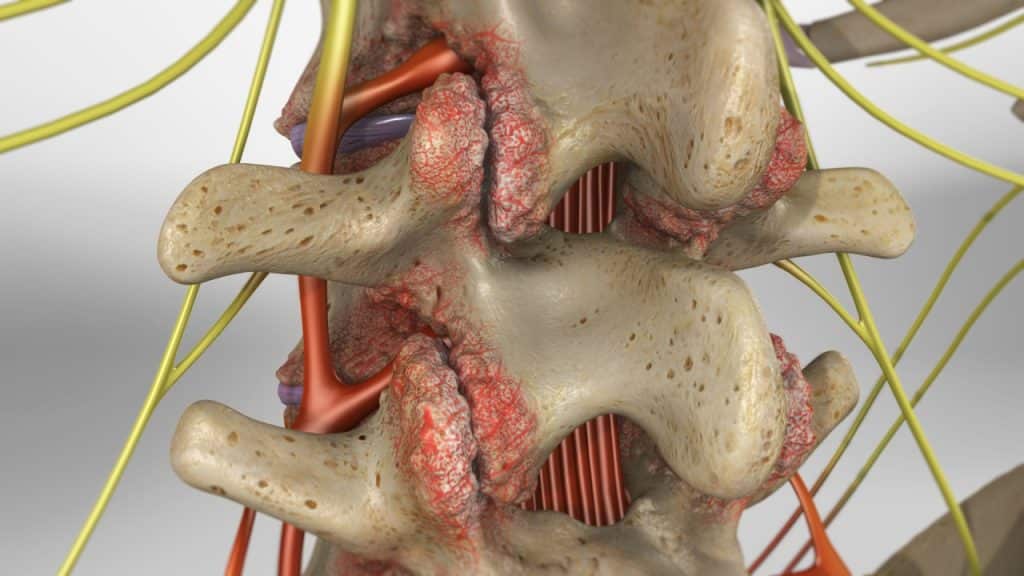
3. Breakdown of Cartilage between the Facet joints – Facet Joint Disease
As the space between the two vertebrae above and below the affected disc gets smaller, there is less padding between them, and the spine becomes less stable. The facet joints, the areas where the vertebrae touch, are forced to shift which can affect their function. The cartilage that covers the stressed facet joints gradually wears away. The joints become swollen and stiff. The vertebral bones rub directly against each other, which can lead to growth of bone spurs along the edges of the facet joints and an enlargement of the joints. Facet joint disease occurs when these joints become stressed and damaged.
4. Bone Spurs Formation
Furthermore, the body can react to the closing gap between the two vertebrae by building osteophytes or bone spurs, small bony projections that develop along the edges of bones. Bone spurs can put pressure on the spinal nerve roots or spinal cord, resulting in pain and affecting nerve function.
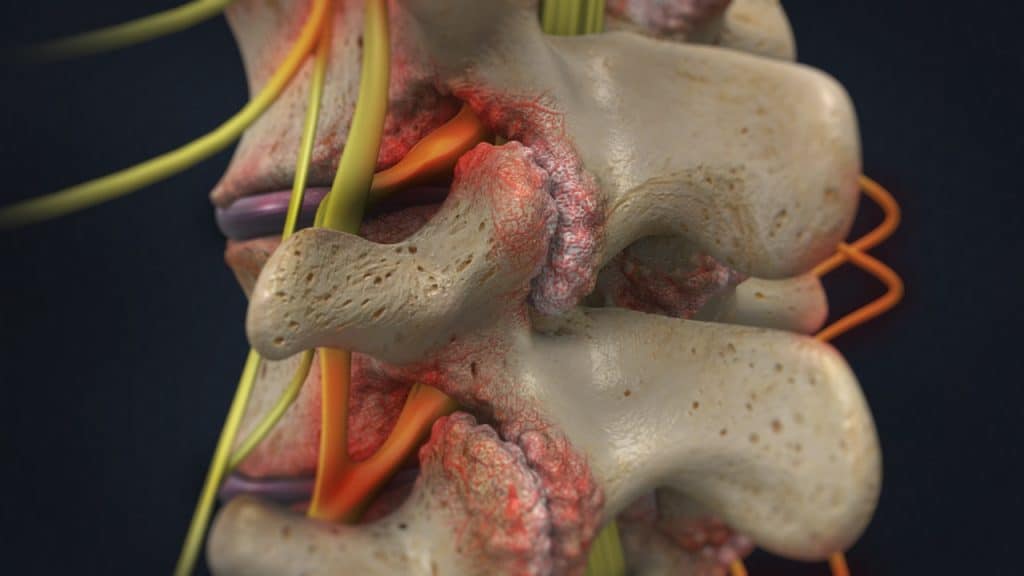
5. Spinal Stenosis
The vertebral shifting and the excess growth of bone (bone spurs or osteophytes) can reduce the space through which the nerve roots travel, and the spinal cord or the nerve roots can become harmfully compressed.
Symptoms
Pain arising from the facet joints varies depending on which region of the spine is affected. If the cervical or upper spine is affected, pain may be experienced in the neck, shoulders and upper or middle back. It can also be accompanied by headaches. If the lumbar spine is affected, pain may be experienced in the lower back with radiation into the buttocks, groin, lower abdomen and back of the thigh.
In cases of spinal stenosis, the symptoms can vary depending on the location and severity of the stenosis in the spine. An affected spinal nerve in the lower back may result in pain, tingling, numbness and/or weakness that radiates from the lower back into the buttocks and legs. An affected spinal nerve in the neck area may causes pain, tingling, numbness and/or weakness that radiates from the neck into the distribution of the affected nerve root in the shoulders, arms or hands.
Treatment
Treatment for painful degenerative disease focuses on minimizing pain, stabilizing the spine, and improving or maintaining mobility. It can usually be treated successfully without surgery with a combination of rest, step positioning (stress-reducing positioning), heat therapy, analgesic/anti-inflammatory medications and physical therapy.
Facet joint infiltrations or facet joint blocks may be administered not only to diagnose facet joint pain but also to treat it. If the patient shows a positive response to the facet joint blocks after having failed nonoperative care, the next treatment option is often radiofrequency denervation or rhizotomy. In unusually chronic, severe and persistent facet joint problems, bone fusion surgery may be an option.
Treatment options for spinal stenosis depend on the location and severity of the injury. The spinal stenosis can usually be treated successfully without surgery with a combination of pain management techniques, physical therapy and therapeutic spinal injections. Surgery may be recommended if the conservative therapies do not alleviate pain and the quality of life is still affected or if a significant neurologic deficit such as progressive muscle weakness exists.
References
- Kraemer J., Hasenbring M., Kraemer R., Taub E., Theodoridis T., Wilke H.J.: Intervertebral Disc Diseases: Causes, Diagnosis, Treatment and Prophylaxis. Thieme 2009.
- Laplante B., DePalma M.: Spine Osteoarthritis. American Academy of Physical Medicine and Rehabilitation 2012; 4: 28-36.
- Kalichman L., Hunter D.: Lumbar Facet Joint Osteoarthritis: A Review. Semin. Arthritis Rheum 2007; 37(2): 69-80.