Basic Principles
Therapeutic spinal injections are highly specialized and effective forms of therapy in the treatment of degenerative diseases of the spine. These are minimally invasive “single-shot”-techniques, in the form of epidural injections, nerve root blocks, facet joint infiltrations and sacroiliac joint infiltrations.
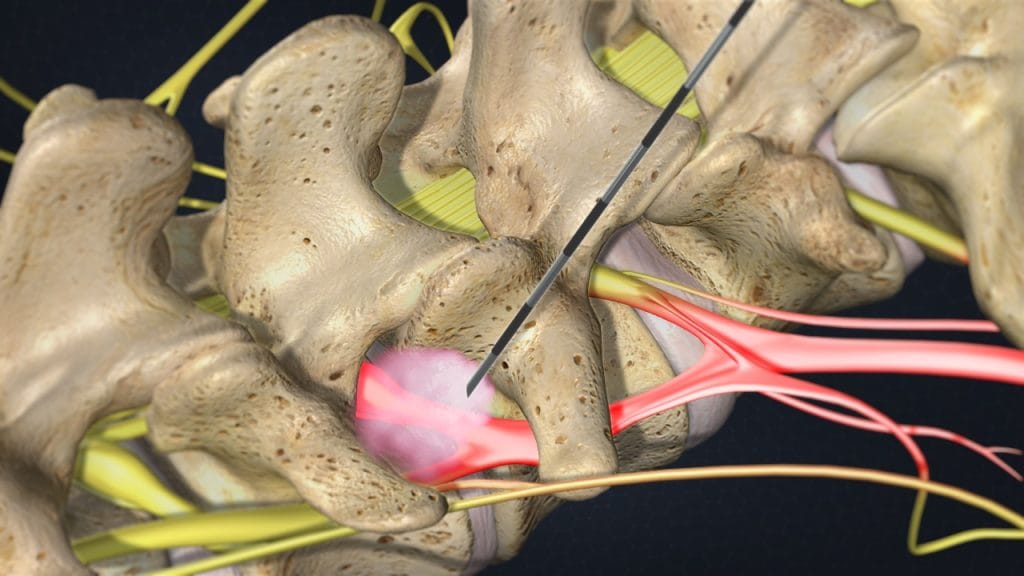
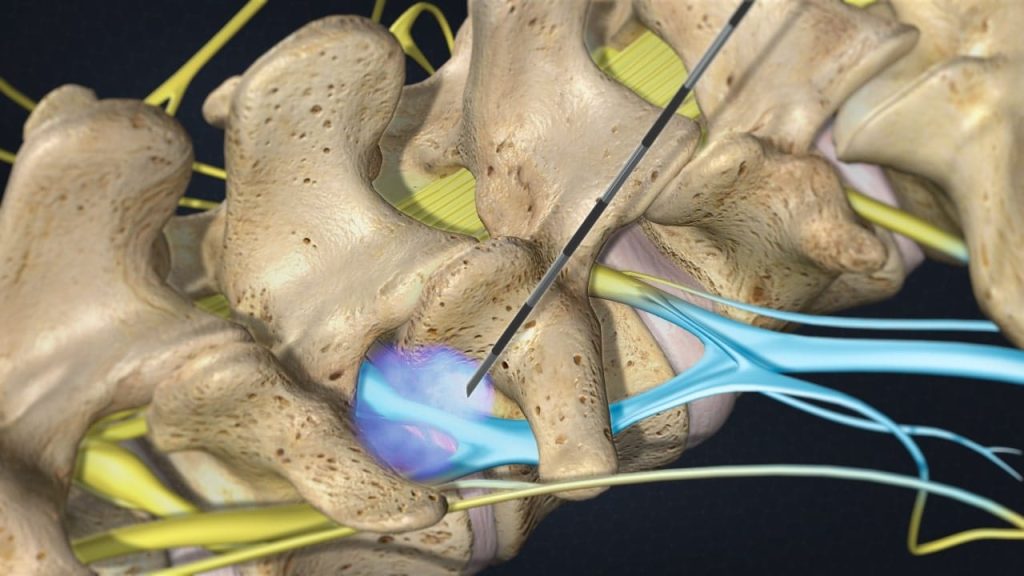
It is possible to treat the primary disorder by injecting fluids with anaesthetic, anti-inflammatory and anti-edemic properties directly into the area that is the source of pain in the spine (nociception area). This avoids loading the entire body with more medication than necessary.
For the therapeutic local injections are mainly used local anaesthetics at low concentration while steroids or a combination of both are rarely used, depending on the purpose of the treatment.
The use of corticosteroids is not mandatory. It should also be noted that their local application to nerve structures (epidural and/or perineural) is an “off-label” use. In addition, some double-blind randomized prospective studies did not demonstrate a clear advantage of combined local anaesthetic/corticosteroid injections versus local anaesthetic injections alone.
The Orthokine technique (serum enriched with Interleukin-1- Receptor Antagonist Protein, IL-1-Ra) offers an alternative form of therapy of nerve root compression syndromes, especially of nerve root irritation caused by postsurgical scarring (failed back surgery syndromes).
Therapeutic local anaesthesia is a fundamental part of the therapeutic local injection treatment. A few millilitres of local anaesthetic at low concentration (0,5%) are enough to switch off sensitized nociceptors (pain receptors) and nerve fibers that have been transformed into nociceptors. This results in the following effects:
- Pain reduction
- Decreased nerve excitability
- Increased irritation thresholds
- Desensitization
- Increased local blood flow
A repeated infiltration of local anaesthetics into the area of nociception and the outgoing afferent nerve fibers results in a desensitization of hyperactive neural elements. It is possible to obtain a permanent effect with a series of 6-12 infiltrations on consecutive days.
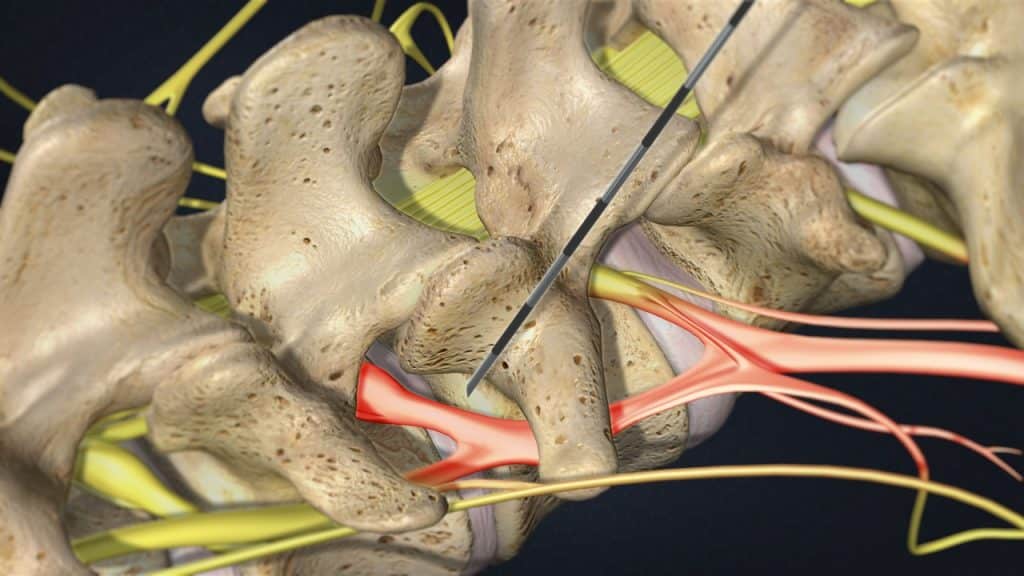
The utility of a minimally invasive spine treatment with repeated nerve root blocks has been investigated in the past years by neurophysiological tests and has proven to be successful in the clinical practice. Experimental studies have shown that inflammatory changes of the nerve root, caused by mechanical compression, can be largely prevented by lidocaine injections. The reduction of edema of the inflamed and swollen nerve root and perineural tissue results in a relative widening of the space within the spinal canal.
Numerous studies in the medical literature have shown that intervertebral disc protrusion and prolapse, spinal canal stenosis and postsurgical scarring may be present without causing any discomfort – they are compensated. One of the essential tasks of the treatment is to restore the state of compensation. This effect can be enhanced by physical therapy, electrotherapy, heat therapy and proper body posture.
Mechanism of action
1. Decreased nerve excitability – Increased irritation thresholds
An action potential is the mode through which a neuron transports electrical signals. Action potential generation is the process by which a neuron rapidly depolarizes from a negative resting potential to a more positive potential and is achieved by influx of cations (sodium or calcium ions) through ion channels.
Local anaesthetics reversibly block nerve conduction near their site of administration, thus producing temporary loss of sensation at a local level. Nerve impulse conduction is blocked by inhibition of sodium channels at the nerve endings and along the axon which transmits the nerve signals. This causes a decrease in nerve cell membrane permeability to cations, especially sodium ions, possibly by competing with calcium-binding sites that control sodium permeability. This change in membrane permeability results in decreased depolarisation and increased excitability threshold that eventually prevents the generation of nerve action potential.
2. Desensitization
Repeated infiltration of local anaesthetic into the area of nociception and the outgoing afferent nerve fibers, which convey sensory signals to the brain, results in a desensitization of overactive neural elements.
Repeated administration of therapeutic local anaesthesia prevents the development of chronic pain. If pain chronification is already developed, repeated therapeutic local anaesthesia disrupts the vicious circle of nociception (the perception of a painful stimulus), muscle spasm and abnormal posture.
3. Increased local blood flow
Most local anaesthetics promote the dilatation of blood vessels (act as vasodilators) and consequently markedly increase the blood flow in the infiltrated area. Subsequently, the local anaesthetic is being removed faster by the circulatory system.
A maximum of 10ml of local anaesthetic at low concentration ((i.e. Meaverin: Mepivacaine 0,5%) is used at each injection session in order to avoid elevated blood level and systemic side effects.
Indications
The main indications for a therapeutic local injection treatment are cervical and lumbar nerve root compression syndromes. They are seen especially as a result of intervertebral disc protrusions/ prolapses, spinal canal stenoses, or postsurgical scarring (failed back surgery syndromes). Often a combination of these causes is present. Further indications are cervical and lumbar facet syndromes, spondylolisthesis and synovial cysts.
Injection Techniques
Therapeutic spinal injections fall into the category of interventional procedures. These can be carried out using non-imaging-/landmark-supported or imaging-supported techniques. Imaging-supported procedures can be performed under ultrasound-, X-ray fluoroscopy-, CT- and rarely MRI-guidance.
1. Anatomical landmarks–guided
The spinal injections can be performed without the aid of imaging techniques, as they can be effectively guided by the palpation of anatomical landmarks. Landmark-guided injection treatments in the spine (as single-shot techniques) are a fast-acting and efficient treatment when carried out by a trained and experienced professional and can be performed at an early stage in an out-patient setting. Generally, they are so beneficial that no further, more invasive measures are required.
The injections are carried out according to specific, predetermined angle and length measurements. These measurements may be additionally verified, prior to carrying out the injection, on the basis of the available diagnostic imaging (MRI- or CT-scan).
The interventional treatment is performed without significant manipulations and thus with minimal hygiene risks. Injections are primarily carried out without the use of ionizing radiation. This enables the repetition of these specific injection therapies at regular intervals, without negative impact on the patient.
2. Ultrasound-guided
Ultrasound-guided injections in the spine can also be carried out with a high degree of efficiency and without ionizing radiation. Limitations of this technique relate to particular anatomical features, regarding the limited possible depth of the injection when using ultrasound imaging.
3. Fluoroscopy or CT-guided
Fluoroscopic or computer tomography (CT) guidance should be used in the initial procedure if the anatomy is in any way atypical, making it difficult to use palpated anatomic landmarks in order to identify the proper injection site. This is the case in the presence of severe scoliosis, transitional vertebrae or obesity.
Fluoroscopic or computer tomography (CT) guidance may also be required for diagnostic purposes prior to nerve root decompression surgery, in order to identify and visualize the affected nerve root, by injection of a contrast dye and an analgesic.
Fluoroscopic guidance is also advisable for intradiscal injections as well as radiofrequency procedures.
It is also necessary to use an imaging technique for any cervical epidural procedure, due to the close proximity to the central nervous system.
4. MRI-guided
MRI-guided injection techniques are less frequently employed in comparison with the other techniques. Non-magnetic cannulas must be used during these procedures and have a greater risk of breaking, as well as being significantly more expensive.
Depending on the treatment goal, the following distinctions are made:
- Perineural techniques (cervical-, thoracic-, lumbar- spinal nerve analgesia).
- Ιnterlaminar epidural techniques (epidural-perineural, epidural-dorsal).
- Transforaminal epidural techniques
- Epidural-sacra
- Periarticular techniques (cervical-, thoracic-, lumbar- facet injections/blocks, sacroiliac joint injections/blocks)
As part of minimally invasive intensive therapy of the spine for the treatment of nerve-root symptoms, a combination of periarticular techniques (e.g. sacroiliac joint or facet injections) may also be possible, in addition to the perineural techniques (e.g. lumbar spinal nerve analgesia).
Out-Patient – In-Patient Treatment
Minimally invasive spine treatments can be carried out in an out-patient or in-patient setting. Apart from a few interventions that require 24-hour monitoring, such as cervical epidural injections, all other interventions can be performed on an out-patient basis. However, in complex, therapy-resistant cases an in-patient treatment can be considered.
Most often, symptoms improve in the long term, so that a further therapy escalation is not necessary. Surgery is recommended in case of a significant neurologic deficit such as progressive muscle weakness. Cauda equina syndrome is a medical emergency that calls for urgent surgical intervention. Most cases of myelopathy will require an operation to relieve pressure on the spinal cord.
Multimodal Program
The minimally invasive spine therapy can be part of a multimodal medical treatment. This concept comprises additionally to minimally invasive interventions (therapeutic spinal injections), pharmacotherapy, psychotherapy, postural and behaviour training (back school) as well as special physical therapy, which includes – among others- exercise, muscle strength training, heat- and electrotherapy. The multimodal medical program is evidence based and specifically recommended by the Drug Commission of the German Medical Association.
Physiotherapy – Exercises
Following minimally-invasive intensive therapy, pain is reduced for the majority of patients to a level where surgery is no longer necessary. Additional treatments such as physiotherapy, electrotherapy, heat therapy and correct positioning to ensure the nerve root is not under stress, all amplify this effect. (Position for reduction of stress: the patient lies on their back in a relaxed position with an approx. 90° angle at hip and knee joints, with the calves resting on an orthopaedic block).
As complaints improve, physiotherapy and a set of exercises are followed to achieve a posture which relieves stress; later still, exercises involving movement are used as part of a medical training programme, alongside individual sports and exercises regimes: with more exercise, pain is reduced. There is evidence to show that physiotherapy exercises, as well as following a programme of general exercise, further stabilize the improved health achieved.
It is absolutely vital that only exercises that do not cause any increase in pain are used (movement in a pain-free space). This means that movement should occur in parts of the body unaffected by the pain. The focus here, however, is on dynamic “moving-forwards sports”, such as swimming, running or cycling. Generally, static cycling machines cause no additional complaints, even in cases of severe pain syndromes associated with the spine.
Studies have shown that in cases of vertebral complains, movement is better than bedrest. Venous flow in the spinal canal is promoted by following an appropriate exercise routine and sporting activities. Furthermore, regular changes between stressing and unstressing of the spine means the spinal disk tissue is better nourished.
References
- Theodoridis T., Kraemer J.: Injektionstherapie an der Wirbelsäule. Manual und Atlas. 3. Auflage. Thieme 2017.
- Theodoridis T., Randel U., Georgallas C.: Landmarkengestützte Injektionstechniken an der Wirbelsäule. Orthopädische und Unfallchirurgische Praxis 2019; 8: 528-539.
- Theodoridis T., Randel U., Georgallas C.: Interventionelle Wirbelsäulentherapie ohne Zuhilfenahme bildgebender Verfahren. Orthopädische und Unfallchirurgische Praxis 2023; 5: 200-206.
- Kraemer J., Hasenbring M., Kraemer R., Taub E., Theodoridis T., Wilke H.J.: Intervertebral Disc Diseases: Causes, Diagnosis, Treatment and Prophylaxis. Thieme 2009.
- Kraemer J., Koester O.: MR Imaging of the Lumbar Spine. A Teaching Atlas. Thieme 2002.
- Kraemer R., Theodorides T., Kraemer J.: Die lumbale Spinalkanalstenose. Springer 2011.
- Yukawa Y., Kato F., Suda K., Yamagata M., Ueta T.: Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine. Part I: Radiographic data from over 1.200 asymptomatic subjects. European Spine Journal 2012; 21(8): 1492-1498.
- Kato F., Yukawa Y., Suda K., Yamagata M., Ueta T.: Normal morphology, age-related changes and abnormal findings of the cervical spine. Part II: Magnetic resonance imaging of over 1.200 asymptomatic subjects. European Spine Journal 2012; 21(8): 1499-1507.