Overview
Lumbar radiculopathy, also called sciatica, is a disease involving dysfunction of one or more nerve roots in the lumbar spine that typically manifests as pain radiating from the lumbar region into the leg, in the area supplied by the affected nerve root. It can be accompanied by sensory, motor, or reflex disturbances.
Any condition that somehow compresses or irritates a lumbar nerve root can cause lumbar radiculopathy. Herniated disc with nerve compression, degenerative disease in the lumbar spine, foraminal stenosis or spinal canal stenosis, scar tissue from previous spinal surgery that is affecting the nerve root, among others, may cause irritation or inflammation of the nerves as they leave the spine area.
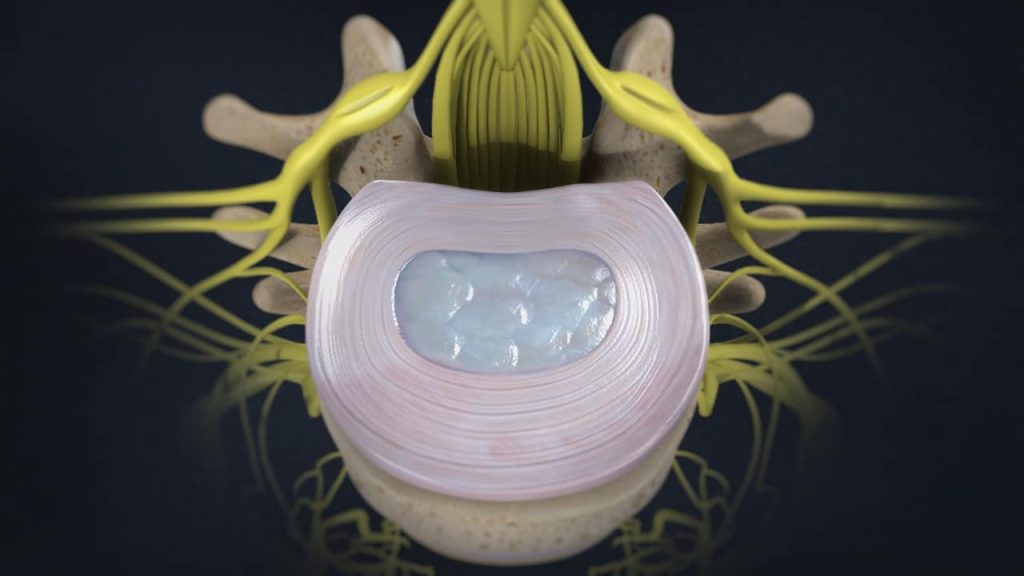
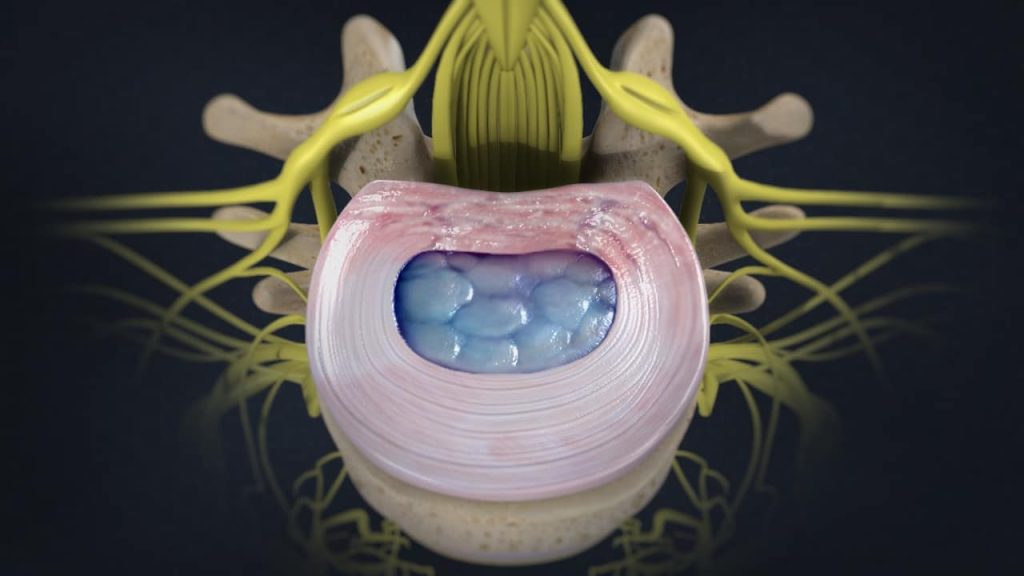
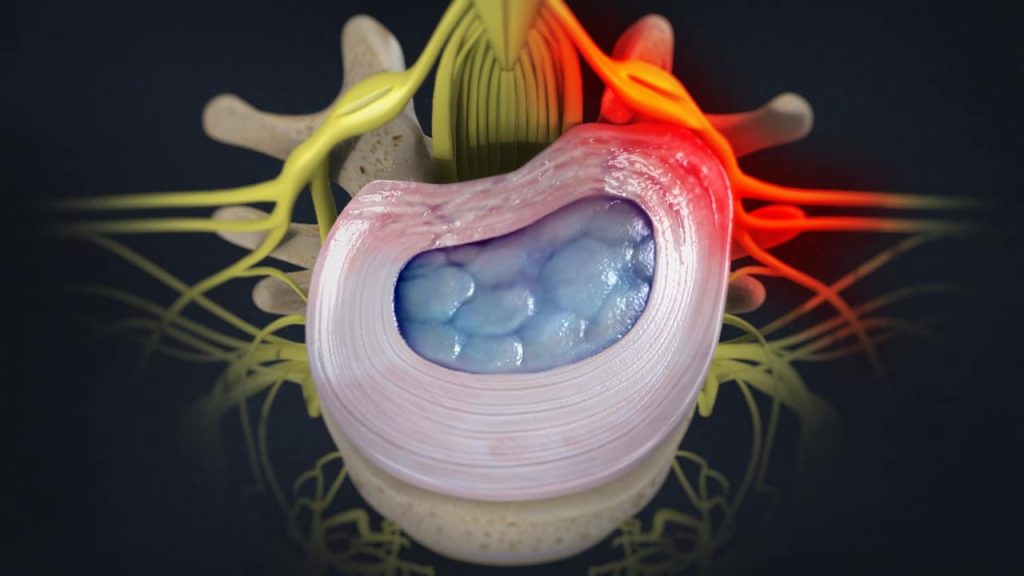
Causes (Lumbar Herniated Disc)
A herniated disc with nerve compression is by far the most common cause of lumbar radiculopathy. A herniated disc can allow disc material to press harmfully against nearby nerve roots, triggering back pain and possibly pain and nerve symptoms such as tingling, numbness, and/or weakness down the leg.
Causes (Degenerative Disc Disease)
Another common cause of nerve root injury is a degenerative disc disease. Degenerative disc disease is an age-related condition that happens when one or more of the discs deteriorate or break down, allowing vertebral bones above and below the disc to shift out of position. The bones can touch, pinching nearby nerve roots, leading to pain and possibly accompanying neurological symptoms such as pins-and-needles tingling, numbness, and/or weakness in the areas served by the affected nerve roots.
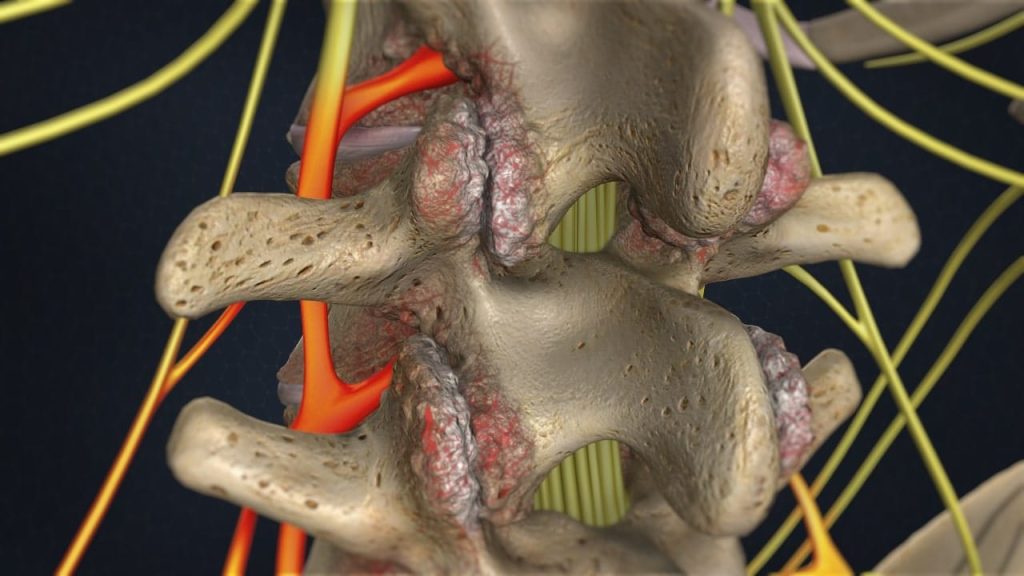
Causes (Lumbar Foraminal Stenosis, Spinal Stenosis)
When a foramen (bony opening where a nerve root exits the spinal canal) or the spinal canal (bone channel occupied by the spinal nerves or the spinal cord) narrows and becomes smaller, the nerve root has less space and may become impinged.
Degenerative changes related to lumbar osteoarthritis and/or lumbar degenerative disc disease may result in nearby bone spurs (osteophytes), thickening (ossification) of the spinal ligaments, or a disc bulging that creates harmful pressure against the nerve roots.
Causes (Failed Back Surgery)
Failed back surgery syndrome is a recognized medical diagnosis for chronic pain and symptoms that persist after a spinal surgery. Spinal surgery is basically performed to achieve two main goals: 1. Decompress a nerve root that is pinched or 2. Stabilize a painful joint. Failed back surgery syndrome may occur when these goals are not achieved, or when spinal surgery
adversely affects a nerve root or other structure near the operated field.
Lumbar radiculopathy can occur as a result of a recurrent disc herniation with nerve compression, a scar tissue formation with binding or looping of the nerve root by fibrous adhesions, known as epidural fibrosis, and a new onset of foraminal or central spinal stenosis.
Symptoms
Lumbar radiculopathy signs and symptoms differ depending on which nerve root is affected.
Nerve root injury may occur at any of the five vertebrae in the lumbar spine, which are called the L1 through L5, or at the level of the sacrum, the upper portion of which is called S1. Symptoms may include pain, pins-and-needles tingling, numbness, and/or weakness in the areas served by the affected nerve roots.
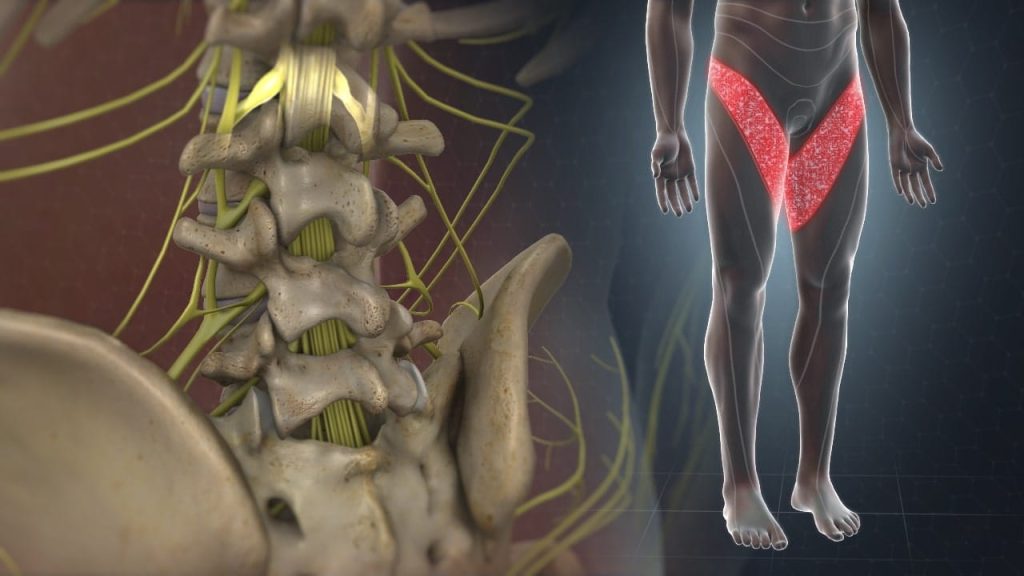
L1 Radiculopathy. Pain, tingling, and/or numbness may be felt from the upper lumbar spine to the groin, over the inguinal dermatome.
L2 Radiculopathy. Pain, tingling, and/or numbness may be felt over the anterior (front) mid-thigh and lateral thigh. Decreased hip flexor strength (hip flexor muscles allow to lift the knee toward the chest) may be experienced.
L3 Radiculopathy. Pain, tingling, and/or numbness may be felt over the inner and anterior (front) lower thigh, never reaching the knee or shin. The knee-jerk reflex (patellar tendon reflex) may be diminished or absent. Weakness and atrophy of the quadriceps muscle (a large muscle group at the front of each thigh) with inability to do a single squat may be experienced.
L4 Radiculopathy. Pain, tingling, and/or numbness may be felt in the area of the knee, the anteromedial shin (front of the leg), and the medial edge of the foot. The knee-jerk reflex (patellar tendon reflex) may be diminished. Weakness and atrophy of the quadriceps muscle with inability to do a single squat may be experienced, but are not as pronounced as in L3 Syndrome.
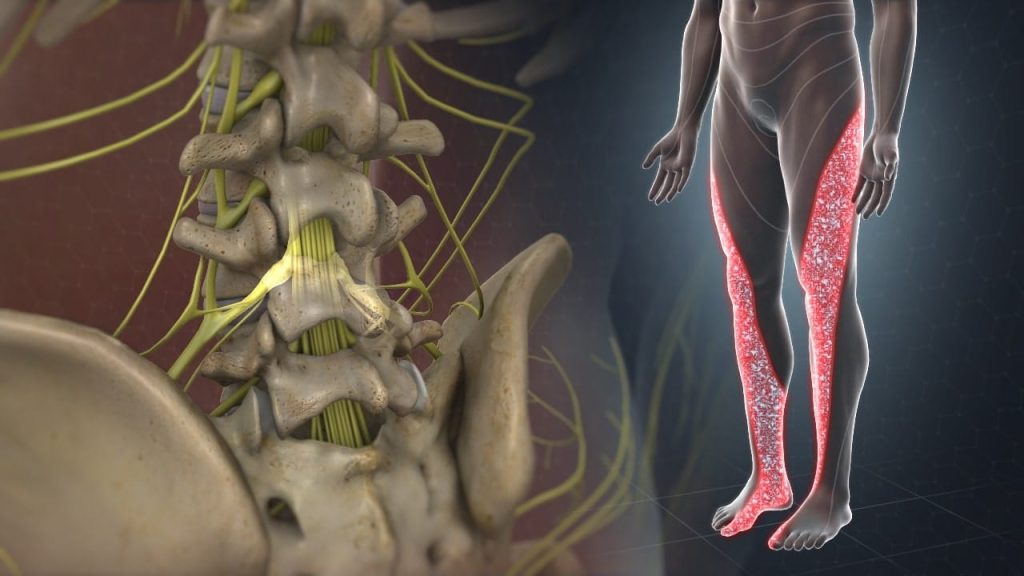
L5 Radiculopathy. Pain, tingling, and/or numbness may be felt down the side of the leg to the top of the foot and great toe. Foot weakness with inability to heel walk and in severe cases a foot and toe drop may be experienced.
S1 Radiculopathy. Pain, tingling, and/or numbness may be felt down the back of the leg and into the heel and/or lateral edge of the foot and the small toe. A characteristic finding is diminution of the Achilles reflex. Foot weakness with inability to toe walk may be experienced.
Treatment
Treatment options for lumbar radiculopathy depend on the location and severity of the injury. Acute lumbar radiculopathy generally has a self-limited clinical course, with a rate of spontaneous improvement of up to a 70-80%. Therefore, nonsurgical treatment is the appropriate initial approach for most patients.
The lumbar radiculopathy can usually be treated successfully without surgery with a combination of pain management techniques, physical therapy and therapeutic spinal injections. Surgery may be recommended if the conservative therapies do not alleviate pain and the quality of life is still affected or if a significant neurologic deficit such as progressive muscle weakness exists.
References
- Kraemer J., Hasenbring M., Kraemer R., Taub E., Theodoridis T., Wilke H.J.: Intervertebral Disc Diseases: Causes, Diagnosis, Treatment and Prophylaxis. Thieme 2009.
- Ropper A., Zafonte R.: Sciatica. Review Article. The New England Journal of Medicine 2015; 372 (13): 1240-1248.
- Baber Z., Erdec M.: Failed Back Surgery Syndrome: Current Perspectives. Journal of Pain Research 2016; 9: 979-987.