Overview
Spinal stenosis is an abnormal narrowing of the spinal canal (bone channel occupied by the spinal nerves or the spinal cord) or of the neural foramen (bony opening where a nerve root exits the spinal canal). This can cause a compression of the nerves or the spinal cord. Spinal stenosis is often the result of degenerative conditions such as osteoarthritis and/or degenerative disc disease. The cervical and the lumbar regions are the parts of the spine which are most commonly affected.
Anatomy
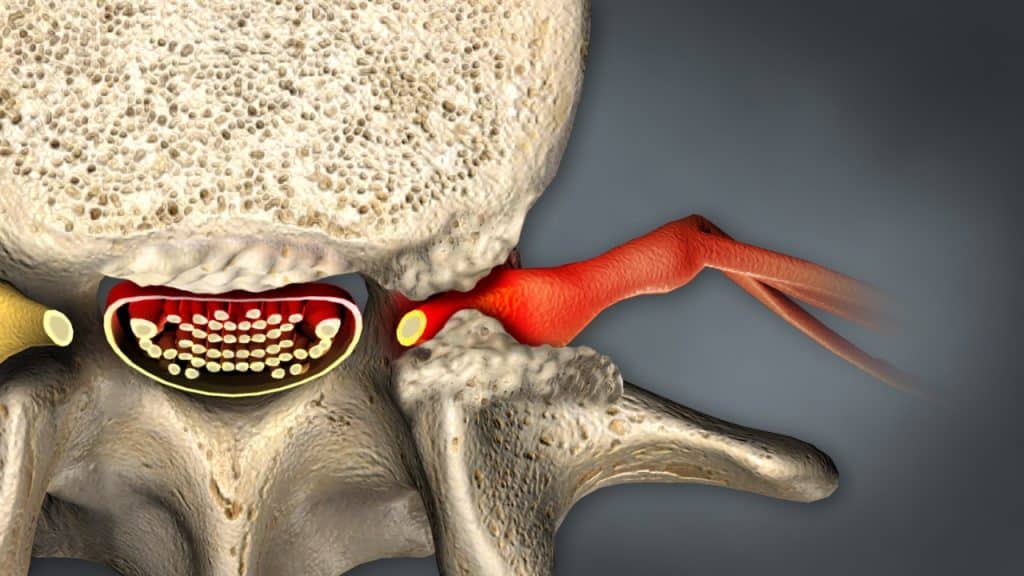
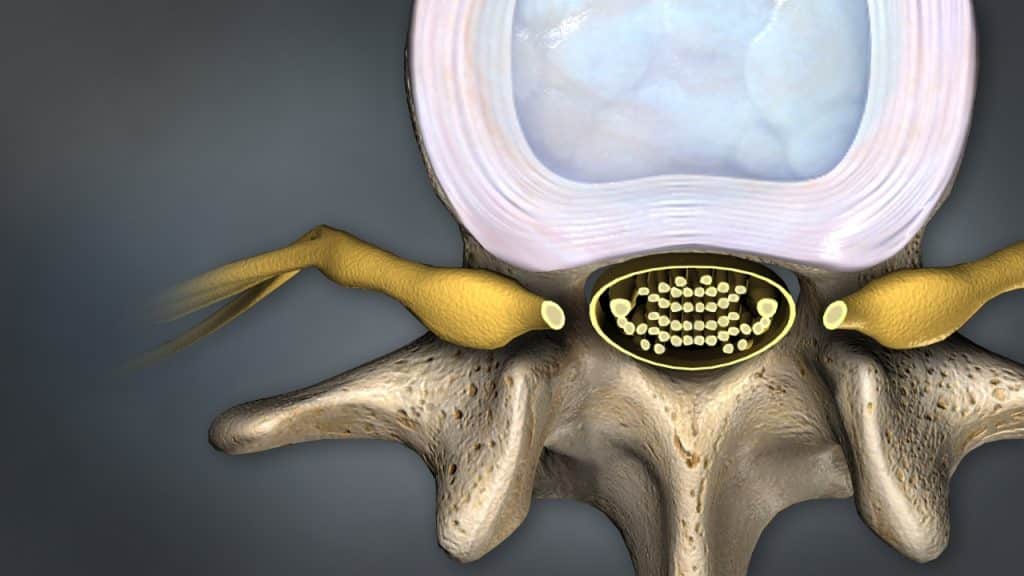
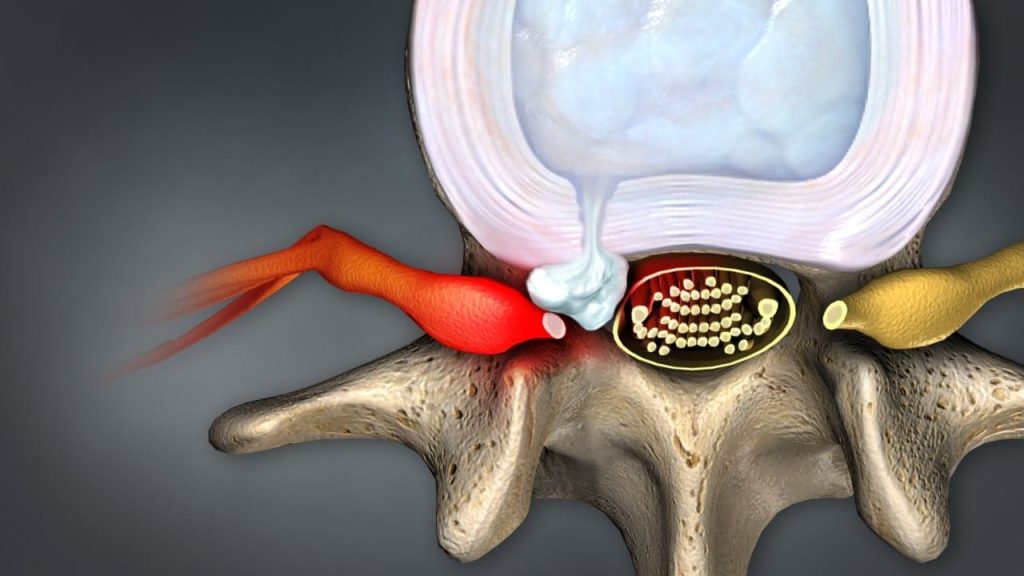
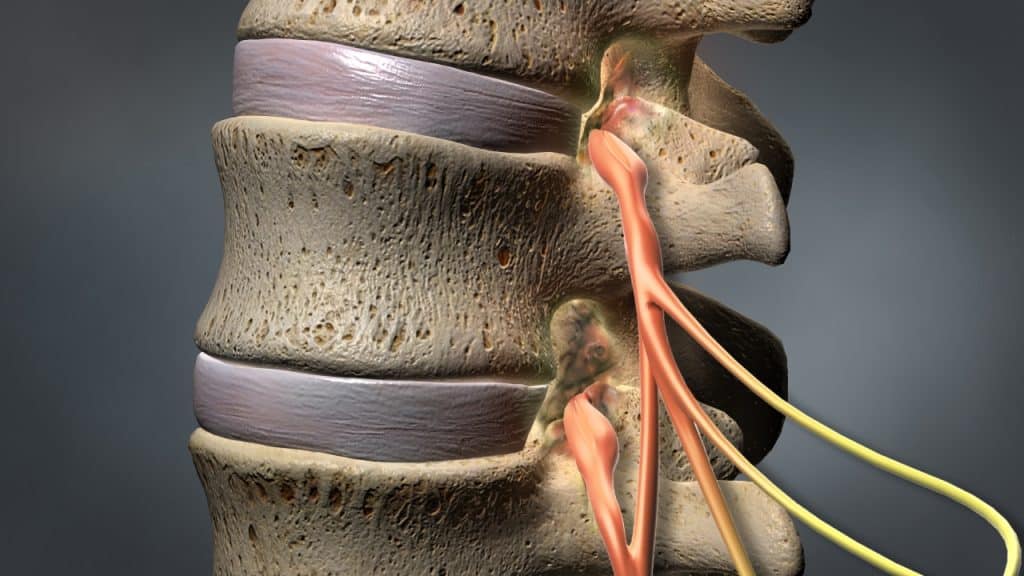
The entire length of the vertebral column has a large central canal or passage, called the spinal canal. In the cervical and thoracic regions of the spine, the spinal cord descends through this space. In the lumbar region of the spine, this space contains a bundle of nerve roots. Openings or holes to each side of the canal, called the neural foramen (intervertebral foramen – foramen between the two adjacent vertebrae) provide pathways for the nerve roots that travel from the spine to other parts of the body.
Stenosis
Normally, there is plenty of room for the nerves in the spinal canal and for the nerve roots as they exit the spine through the neural foramen. With spinal stenosis, however, the space for the spinal cord and/or the spinal nerves is constricted. The spinal nerves can become compressed against the vertebral bone. This can interfere with nerve function.
Causes
Spinal stenosis may be asymptomatic/compensated (without symptoms) or symptomatic/ decompensated (with symptoms). Most cases are asymptomatic but can become symptomatic under certain conditions.
Spinal stenosis is commonly caused by degenerative changes related to osteoarthritis, such as an excess growth of bone (bone spurs or osteophytes) or thickened spinal ligaments such as the ligamentum flavum and the posterior longitudinal ligament, that create harmful pressure against the nerve roots.
Other factors contributing to decompensation and symptoms of spinal stenosis may include herniated discs, abnormal stresses on the spine, dislocation or fracture of the vertebral bone, tumors and postoperative scarring.
In some cases, a person is born with a small spinal canal that does not provide enough room for the spinal nerves.
Symptoms
Symptoms of the spinal stenosis can vary depending on the location and severity of the stenosis in the spine. Generally, spinal stenosis symptoms develop slowly over time and they tend to recur. They usually occur during certain activities such as walking (painful cramping or weakness in the legs during walking, known as neurogenic claudication) and prolonged upright standing for lumbar stenosis (in the upright position the spinal canal gets narrower, worsening the stenosis and pitching the nerve roots in the canal) or biking while holding the head upright for cervical stenosis. The symptoms are often relieved by rest (sitting or lying down) and/or any flexed forward posture, which opens up the spinal canal.
Spinal stenosis in the lower back commonly causes pain, tingling, numbness and/or weakness that radiates from the lower back into the buttocks and legs. In rare cases, the severe compression on the nerve bundle at the end of the spinal cord, known as cauda equina (horse’s tail) can lead to serious problems such as a loss of bowel or bladder function, a condition known as cauda equina syndrome.
Spinal stenosis in the cervical region causes pain in the neck, tingling, numbness and/or weakness that radiates from neck into the distribution of the affected nerve root in the shoulders, arms and hands. In severe cases, the spinal cord compression can lead to serious problems such as extreme weakness, problems with balance and coordination or even paralysis, a condition known as cervical myelopathy.
Treatment
Treatment options for spinal stenosis depend on the location and severity of the injury. The spinal stenosis can usually be treated successfully without surgery with a combination of pain management techniques, physical therapy and therapeutic spinal injections.
Surgery may be recommended if the conservative therapies do not alleviate pain and the quality of life is still affected or if a significant neurologic deficit such as progressive muscle weakness exists.
Cauda equina syndrome is a medical emergency that calls for urgent surgical intervention.
Most cases of myelopathy will require an operation to relieve pressure on the spinal cord.
References
- Kraemer J., Hasenbring M., Kraemer R., Taub E., Theodoridis T., Wilke H.J.: Intervertebral Disc Diseases: Causes, Diagnosis, Treatment and Prophylaxis. Thieme 2009.
- Kraemer J., Koester O.: MR Imaging of the Lumbar Spine. A Teaching Atlas. Thieme 2002.
- Kraemer R., Theodorides T., Kraemer J.: Die lumbale Spinalkanalstenose. Springer 2011.