Overview
Failed back surgery syndrome is a recognized medical diagnosis for chronic pain and symptoms that persist after a spinal surgery, whether to the neck or back.
Spinal surgery is basically performed to achieve two main goals: 1. Decompress a nerve root that is pinched or 2. Stabilize a painful joint. Failed Back Surgery Syndrome may occur when these goals are not achieved, or when spinal surgery adversely affects a nerve root or other structure near the operated field.
Causes (Inaccurate Diagnosis)
The successful outcome of a spinal surgery is dependent on the accurate diagnosis of the patient’s etiology of pain. By far the number one reason for spinal surgery to fail to relieve symptoms, and to possibly create more symptoms, is when the lesion that was operated on is not in fact the cause of the patient’s pain. A possible reason for this is that the spine is a complex entity of numerous structures and mobile joints, and a lot of times the pain is triggered by more than one structure. A huge limitation in spine care is the lack of imaging that can be performed while the spine is in motion or the individual is recreating a motion that triggers the symptoms.
Causes (Altered Biomechanics – Postoperative Instability)
Altered biomechanics from spinal surgery can accelerate the normal, age-related development of the spine within that region. For example, after the surgical removal of a large part of a disc, analogous changes occur very rapidly, so that the adjacent structures lack the time to adapt.
Recurrent Disc Herniation
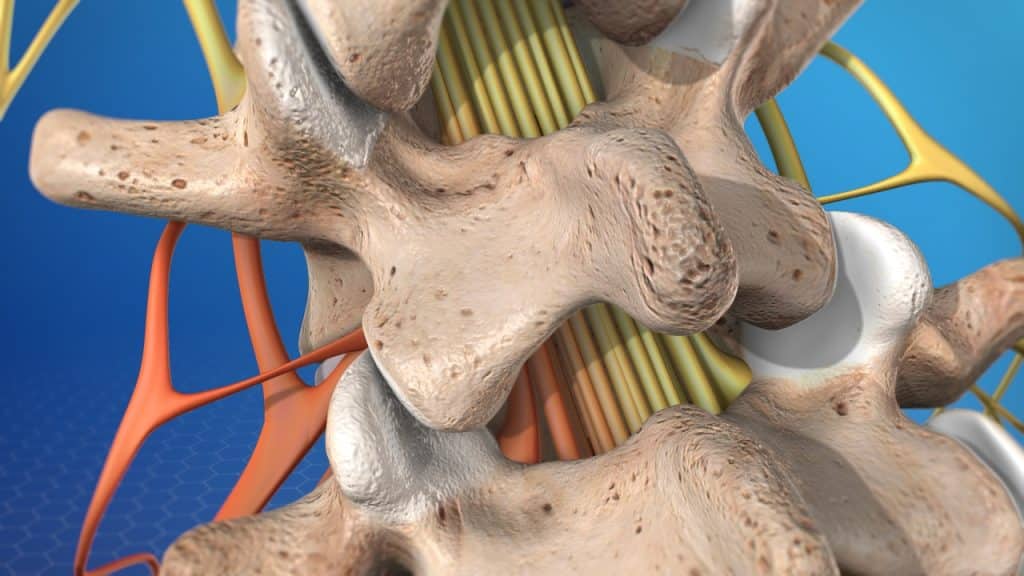
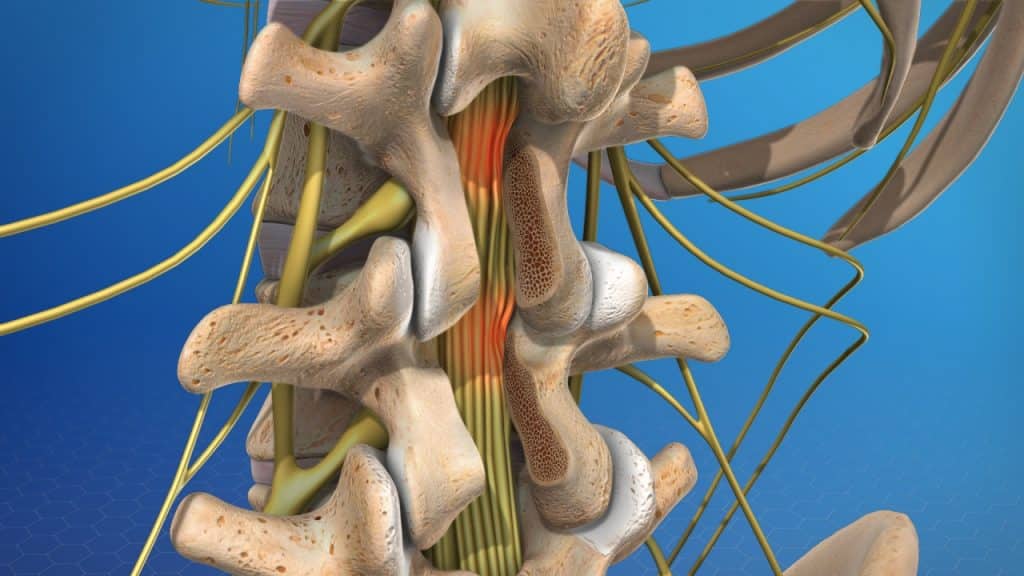
The intervertebral discs are shock absorbers that are located between the bones of the spine, called vertebrae (hence the name intervertebral).
Whenever disc tissue is removed from the intervertebral space, either spontaneously by disc herniation or through surgical extraction, this disrupts the integrity of the disc as an osmotic system. Loss of height and elasticity adversely affect its biomechanical properties, increasing the risk for a recurrent disc herniation.
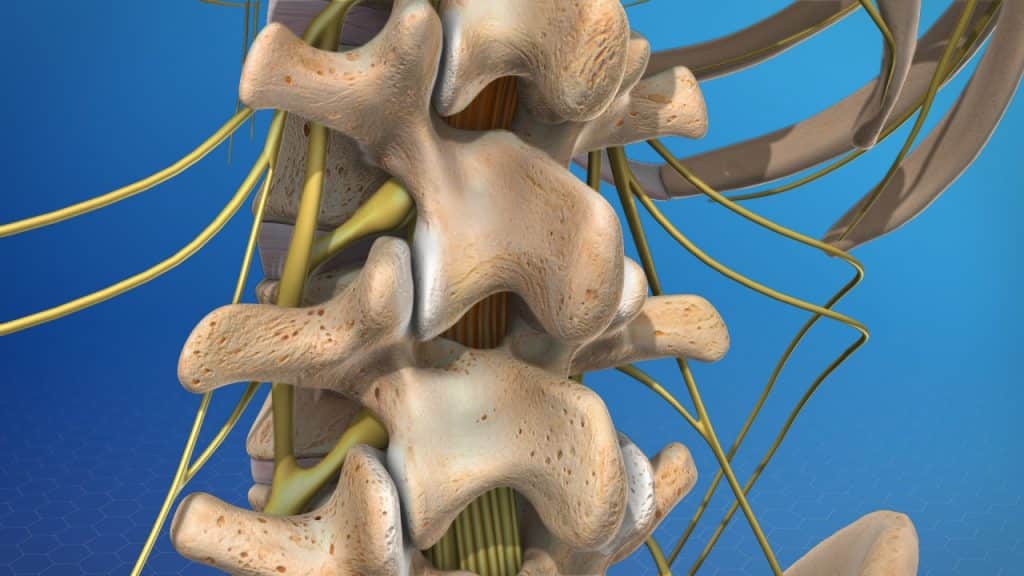
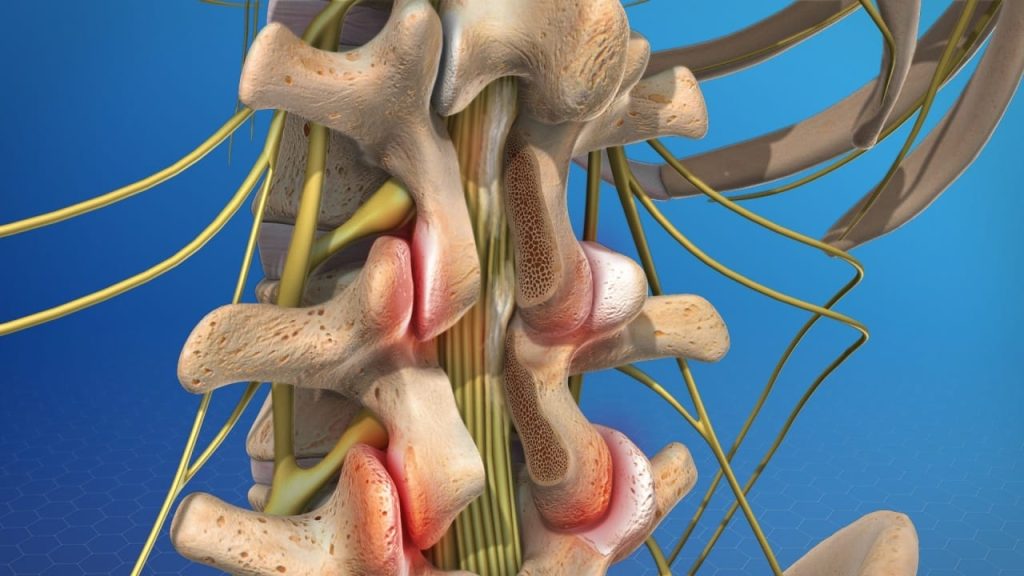
Facet Joint Disease
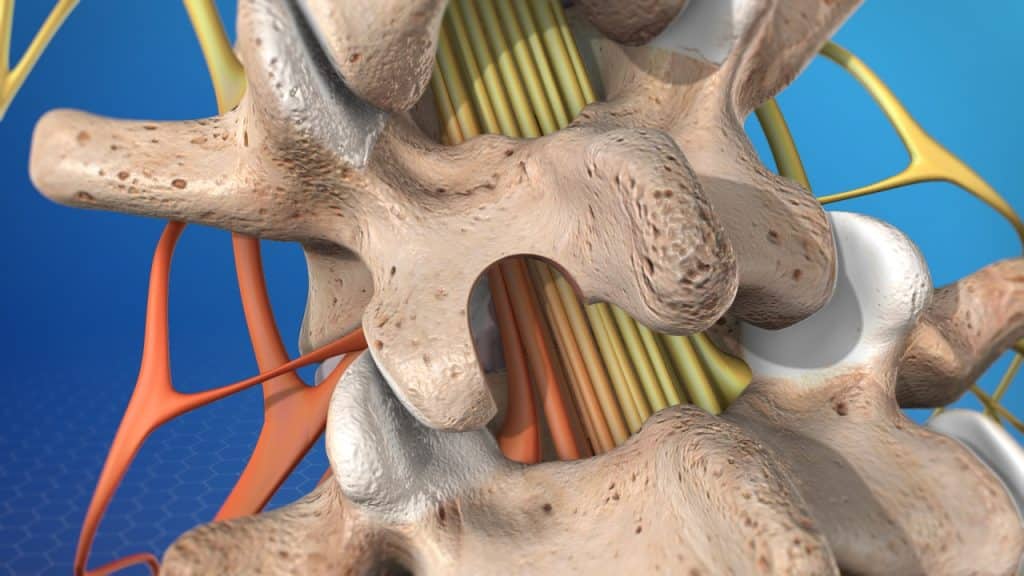
As the space between the two vertebrae above and below the affected disc gets smaller, there is less padding between them, and the spine becomes less stable. The facet joints, the areas where the vertebrae touch, are forced to shift: they become telescoped into each other which can affect their function.
The cartilage that covers the stressed facet joints gradually wears away. The joints become swollen and stiff. The vertebral bones rub directly against each other, which can lead to growth of bone spurs (osteophytes) along the edges of the facet joints and to an enlargement of the joints.
Facet joint syndrome or facet joint disease is a pain arising from the intervertebral joint facets.
Spinal Stenosis
The vertebral shifting and the excess growth of bone (bone spurs or osteophytes) can reduce the space through which the nerve roots travel, and the spinal cord or the nerve roots can become harmfully compressed.
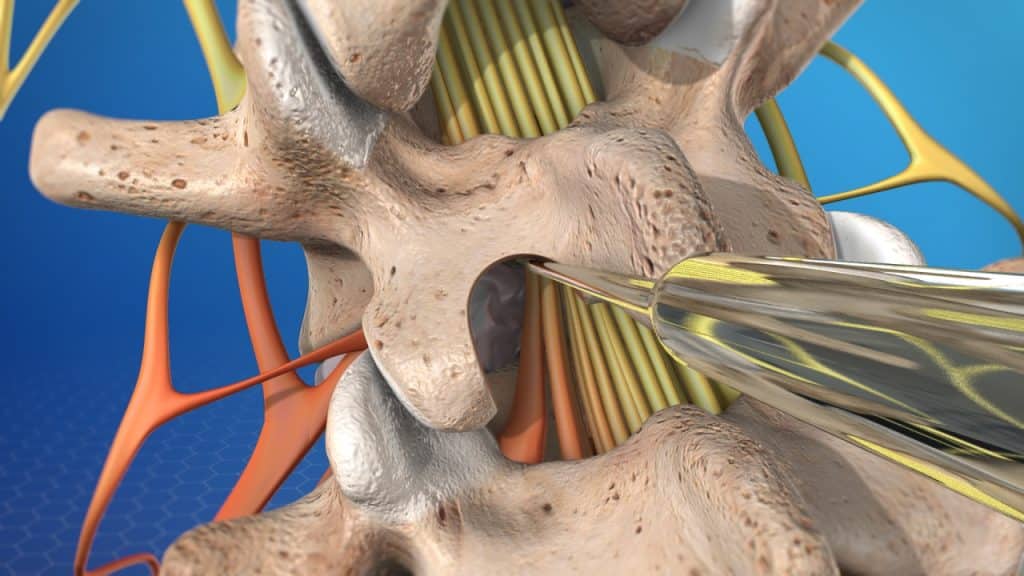
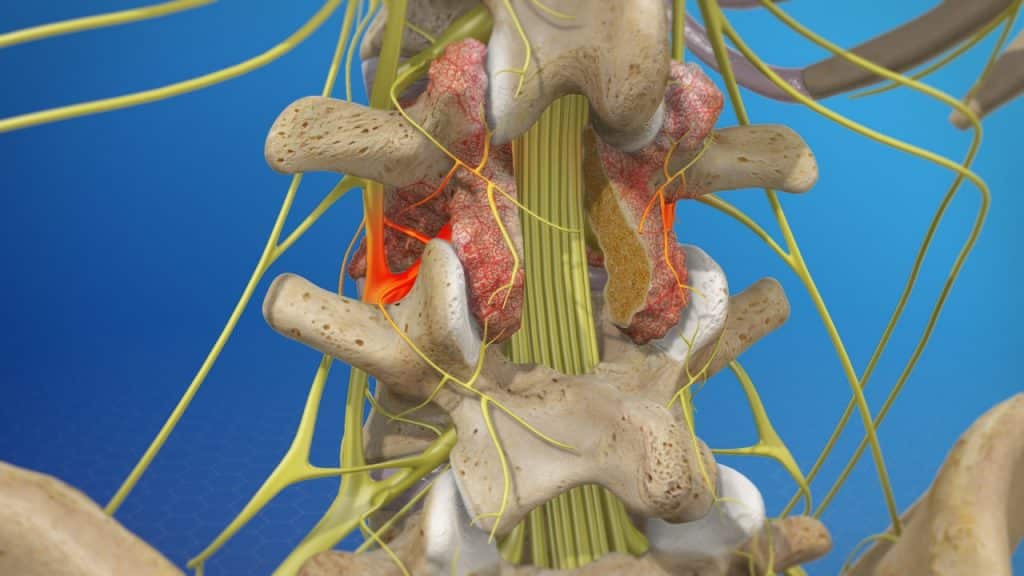
Causes (Scar Tissue Formation – Epidural Fibrosis)
Scar tissue formation is part of the normal healing process after spinal surgery. The extent of postoperative scarring (adhesions) largely depends on the patient’s intrinsic tendency toward scar formation. Additionally, exogenous factors such as surgeries complicated by extensive bleeding or injuries of the nerve root and suboptimal postoperative care may also promote scarring.
While scar tissue can be a cause of pain, actual scar tissue pain is very rare since the tissue contains no nerve endings. Rather, the principal mechanism of pain is believed to be the binding or looping of the nerve root by fibrous adhesions, known as epidural fibrosis.
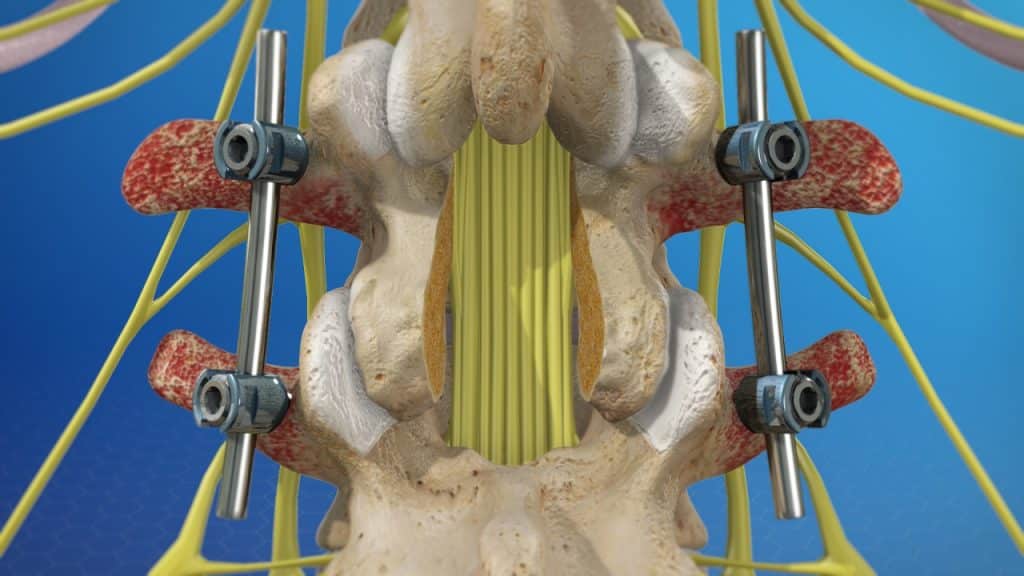
Causes (Fusion Surgery Considerations)
Spinal fusion surgery permanently fuses one vertebral level with another, with the specific intent of stopping movement between the two. This places additional stress on levels above and below the fusion, potentially increasing degenerative changes and pain to these new areas. Additionally, fusion of the lumbar spine to the sacrum as well as fusion of multiple segments may lead to sacroiliac joint disease. Furthermore, fusion surgery has the inherent risk of failure to fuse properly.
Causes (Muscular Deconditioning)
Altered biomechanics from back surgery may result in increased tension on the spine muscles directly controlling movement of the vertebral column. Increased tension on these muscles can lead to stiffness, inflammation, spasms, and fatigue, which may all act to elicit pain in the back.
Symptoms
Symptoms vary depending on the location and which structure is affected. After operations that have been carried out without complication, the typical symptoms tend to arise after an asymptomatic interval of several months. Common symptoms include back or neck pain at the site of the surgery. The pain can be sharp, burning or stabbing and may radiate down to the leg or arm. This pain may feel diffuse, dull and achy. Tingling, numbness and/or weakness may be experienced in the extremities.
Treatment
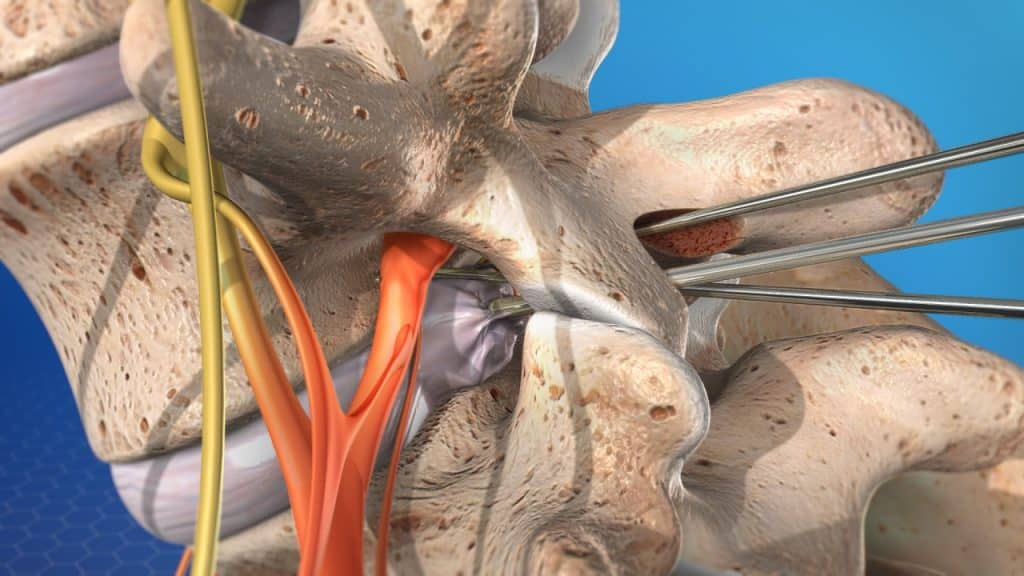
Treatment options for failed back surgery depend on the location and severity of the injury.
The initial mainstays of treatment are a combination of pain management techniques, physical therapy and therapeutic spinal injections.
Surgery may be recommended if the conservative therapies do not alleviate pain and the quality of life is still affected, or if a significant neurologic deficit such as progressive muscle weakness exists.
References
- Kraemer J., Hasenbring M., Kraemer R., Taub E., Theodoridis T., Wilke H.J.: Intervertebral Disc Diseases: Causes, Diagnosis, Treatment and Prophylaxis. Thieme 2009.
- Sebaaly A., Lahoud M-J., Rizkallah M., Kreichati G., Kharrat K.: Etiology, Evaluation and Treatment of Failed Back Surgery Syndrome. Asian Spine Journal 2018; 12 (3): 574-585.
- Baber Z., Erdec M.: Failed Back Surgery Syndrome: Current Perspectives.
Journal of Pain Research 2016; 9: 979-987.