Overview
Discogenic pain is pain arising from a damaged intervertebral disc. It is commonly caused by disc degeneration, an age-related condition. However, this does not necessarily mean that all degenerated discs lead to pain. Discogenic pain is a common reason for chronic lower back and neck pain.
Disc Anatomy
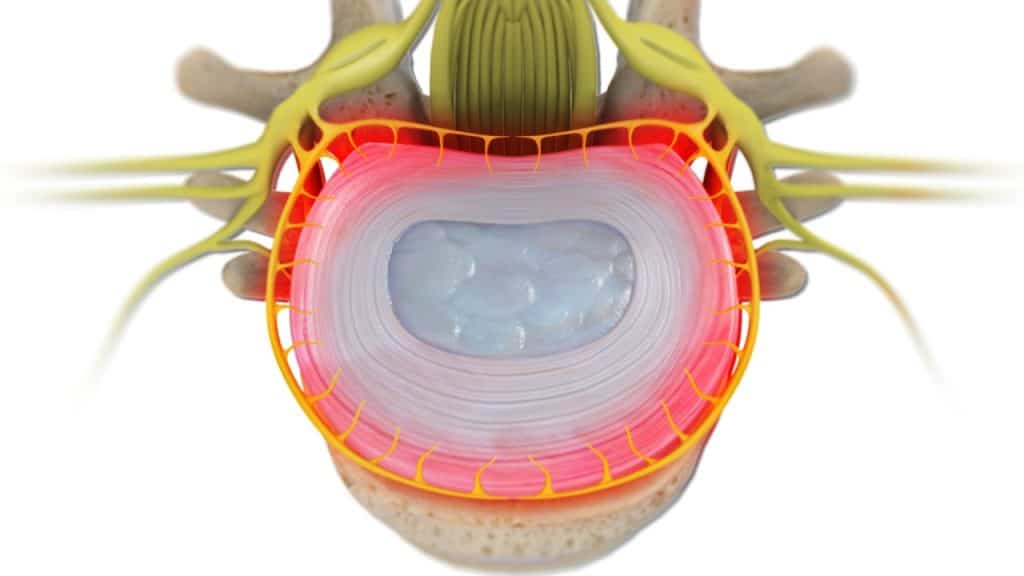
The intervertebral discs are shock absorbers that are located between the bones of the spine, called vertebrae (hence the name intervertebral). They are designed to help the back stay flexible while resisting forces and to allow bending, flexion and twisting of the spine. Each disc has a thick outer layer, known as annulus fibrosus, that surrounds the soft gel-like center, known as nucleus pulposus. A healthy, well-hydrated disc contains a great amount of fluid in its center.
Similar to other parts of the body, each intervertebral disc has a nerve supply. The nucleus pulposus lacks nerve supply. On the contrary, the outer part of the annulus fibrosus contains nerve fibers. Discogenic pain occurs when these nerve fibers are irritated.
Disc Degeneration
1.Loss of Fluid
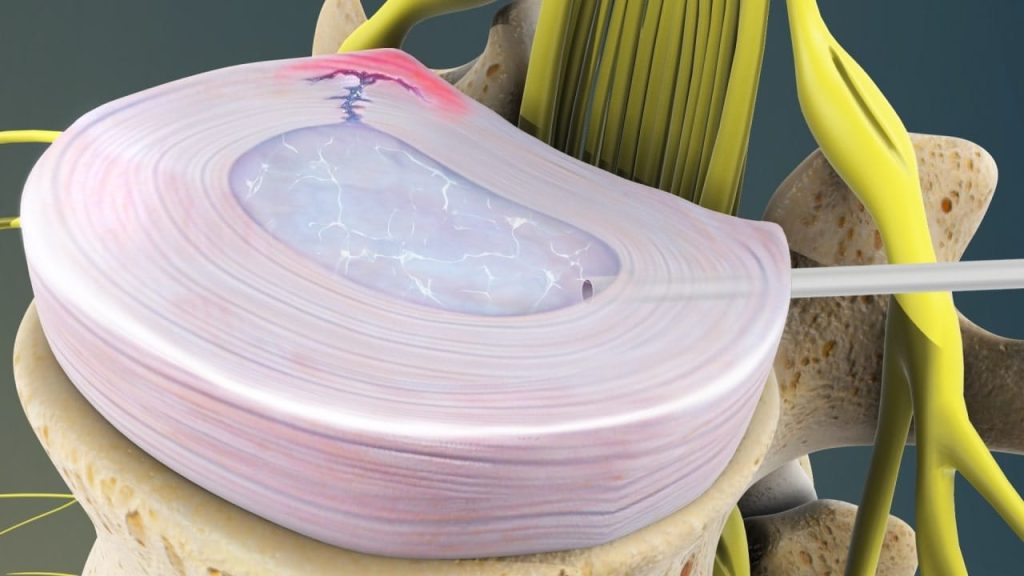
A degenerated disc is marked by a significant decrease in hydration, making the disc less flexible, thinner with narrowing the distance between the adjacent vertebrae and more prone to tearing or cracking in the outer layer of the disc (disc wall), known as annulus fibrosus.
2.Disc Tearing – Disc Healing – Disc Weakening and Collapse
The disc is unable to truly repair itself because it does not have a direct blood supply. Consequently, a tear in the annulus either will not heal or will develop a scar tissue that is not as strong as the original one, having the potential to break again with further disc-weakening and collapse.
Internal Disc Disruption
An internal disc disruption occurs when the disc tears or cracks create pathways for the degenerated nucleus material to leak into the nerve fibers located in the outer part of the annulus fibrosus. The nucleus material contains high levels of inflammatory substances, which leads to an inflammatory response and pain, when it comes in contact with the nerves fibers located in the annulus.
Other contributors to discogenic pain include genetic factors, nutrition and mechanical or traumatic disruption.
Symptoms
Most commonly, discogenic pain is associated with activities or conditions that elevate the pressure within the intervertebral disc, known as intradiscal pressure. These include bending forward, twisting, lifting, sitting, coughing and sneezing.
Early degenerative disc disease may cause no symptoms, but when the degeneration becomes advanced low back or neck pain may occur. The pain can be mild or so intense that the individual cannot follow everyday activities. It can occur suddenly or develop slowly and gradually aggravate over time.
Damage to the annulus can cause chronic low back pain without disc herniation and nerve root compression. Axial back pain represents the most common type of low back pain. It refers to pain that remains within the low back and is usually described as dull and aching. It can also be accompanied by muscle spasms and tightness in the low back, pelvis and hips.
Discogenic pain can also be accompanied by radiculopathy (a disease involving dysfunction of one or more nerve roots as a result of compression or irritation). The pain localization depends on the region of the affected disc. An affected disc in the lower back may result in pain in the back, buttock, or leg, while an affected disc in the neck area may result in neck or arm pain. It can be accompanied by sensory, motor, or reflex disturbances.
Diagnostic Procedures (MRI, Discography)
Magnetic resonance imaging (MRI) is mainly used to diagnose discogenic pain. However, a discography or discogram can also be used to definitely confirm that the pain arises from a specific disc or discs. During this sterile procedure, a contrast dye is injected into each disc under fluoroscopic X-ray guidance. The contrast dye elevates the pressure inside the disc and may provoke the pain of the patient.
Treatment
Treatment for discogenic pain focuses on minimizing pain, stabilizing the spine and improving or maintaining mobility. It can usually be treated successfully without surgery with a combination of rest, step positioning (stress-reducing positioning), heat therapy, analgesic/anti-inflammatory medications, orthopaedic braces and physical therapy.
The lumbar or cervical radiculopathy can usually be treated successfully without surgery with a combination of pain management techniques, physical therapy and therapeutic spinal injections.
Intradiscal electrothermal therapy (IDET) is a minimally invasive procedure used to treat discogenic pain. Under X-ray guidance, a small catheter is placed against the painful part of the disc and heat energy is used to coagulate the fibers of the annulus. The purpose of this procedure is to reduce the sensitivity of the nerves fibers in the spinal disc and to shrink tears or cracks in the outer layer of the disc (disc wall).
Surgery may be recommended if the conservative therapies do not alleviate pain and the quality of life is still affected or if a significant neurologic deficit such as progressive muscle weakness exists.
References
- Kraemer J., Hasenbring M., Kraemer R., Taub E., Theodoridis T., Wilke H.J.: Intervertebral Disc Diseases: Causes, Diagnosis, Treatment and Prophylaxis. Thieme 2009.
- Theodoridis T., Kraemer J.: Injektionstherapie an der Wirbelsäule. Manual und Atlas. Auflage. Thieme 2017.
- Bogduk N.: Practice Guidelines for Spinal Diagnostic and Treatment Procedures. Edition. International Spine Intervention Society 2013.
- Müller F., Veihelmann A.: Radiofrequenz Behandlung in der Schmerztherapie. Indikationen, Techniken, Durchführung.